
The Journey of Opening a Medical Practice: What Every Physician Needs to Know
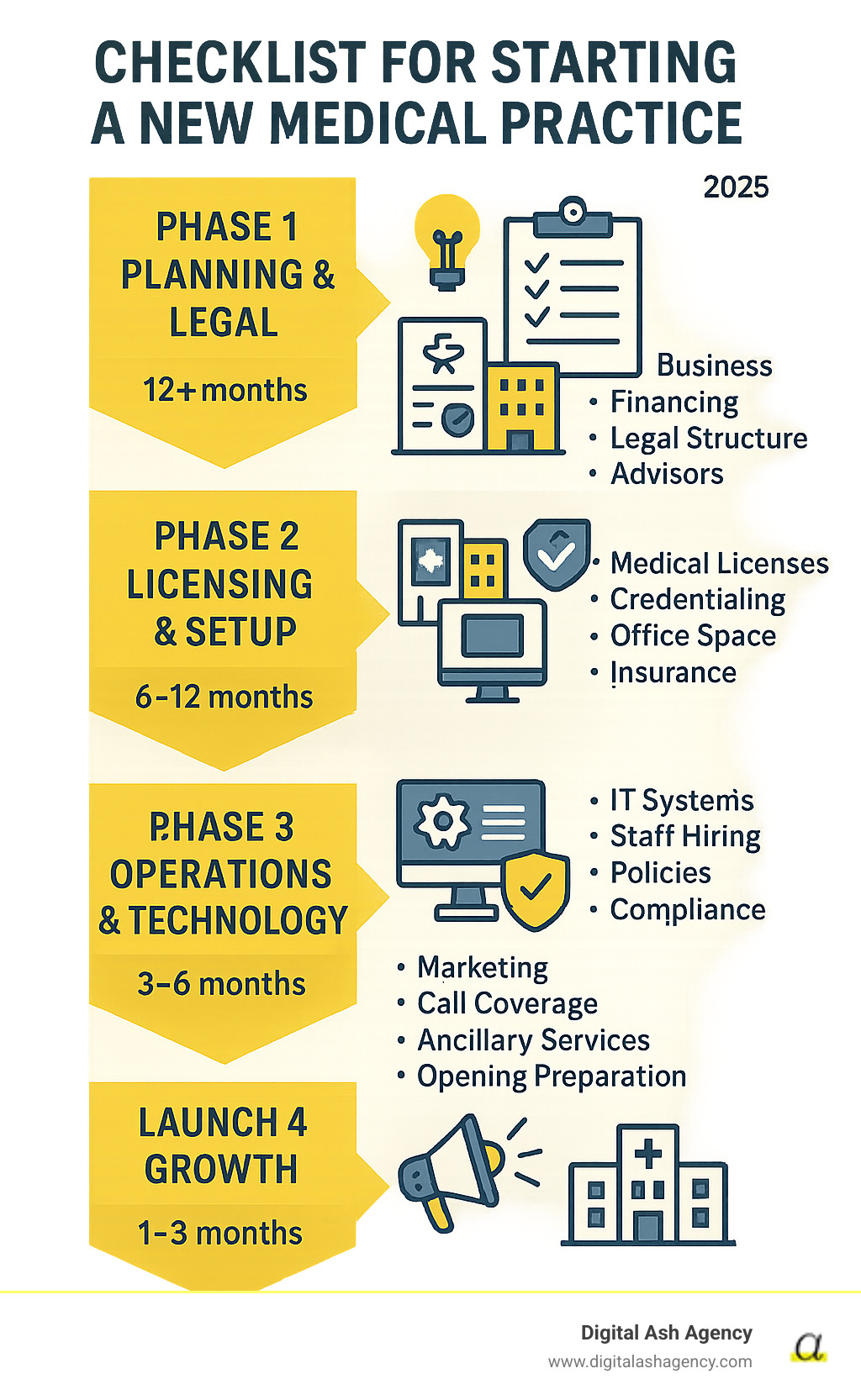
A checklist for starting a new medical practice is your roadmap for turning clinical expertise into a successful business. The process is complex, moving you from physician to entrepreneur managing licenses, staffing, and marketing. It can feel overwhelming, but a structured approach makes it manageable. This guide breaks the journey into four key phases:
- Phase 1: Planning & Legal (12+ months out): Develop a business plan, secure financing, choose a legal structure, and hire advisors.
- Phase 2: Licensing & Setup (6-12 months out): Obtain licenses and permits, complete insurance credentialing, select and design your office, and get malpractice insurance.
- Phase 3: Operations & Technology (3-6 months out): Install IT systems and EMR, hire and train staff, establish workflows, and ensure regulatory compliance.
- Phase 4: Launch & Growth (1-3 months out): Implement marketing, plan for call coverage, consider ancillary services, and prepare for your grand opening.
As one expert notes, "Starting a medical practice... goes well beyond the owner's knowledge of clinical medicine." With proper planning, you can avoid common pitfalls and launch a thriving independent practice.
I'm Ashley Gay, a branding expert who helps physicians steer the startup process, even with non-compete agreements. Using this systematic checklist for starting a new medical practice, my husband's practice billed $239K in its first 90 days. I'll walk you through the critical steps to launch successfully in today's competitive healthcare market.
Phase 1: Foundational Planning & Legal Framework
This initial phase is about creating the blueprint for your practice. Before considering decor or equipment, you must establish a solid legal and financial foundation. This is a critical part of your checklist for starting a new medical practice.
Develop a Comprehensive Business Plan: Your First Step in the Checklist for Starting a New Medical practice
Your business plan is the roadmap guiding every future decision. It's essential for securing loans and defining your strategy. Key components include your mission and vision, target patient demographics, a list of services, and a competitive market analysis. The plan should also cover marketing, operations, management structure, and detailed financial projections. A conservative but realistic financial forecast is crucial; it's wise to overestimate costs and underestimate revenue for the first year. Working with a healthcare consultant or attorney can help you avoid common pitfalls. For more guidance, see our resource on creating a business plan for healthcare and learn the general components of a business plan.
Secure Financing and Manage Your Budget
Starting a practice requires significant capital. First, calculate your startup costs, including rent, initial payroll, EMR software, medical equipment, insurance, and legal fees. Next, project your operating expenses for at least the first year. A crucial tip: have at least six months of operating expenses in reserve, as insurance credentialing and revenue cycles take time. A line of credit to cover 120 days of expenses is a smart safety net.
Financing options include:
- Traditional business loans
- SBA loans
- Specialized medical practice loans
- Equipment financing
- Lines of credit
To save money, consider sourcing equipment from retiring physicians or hospitals with excess inventory.
Establish Your Legal Business Structure
This decision impacts your personal liability and taxes. Always consult a healthcare attorney to choose the right structure for your situation. Common options include:
- Sole Proprietorship: Simple, but offers no liability protection.
- Partnership: For practices with multiple owners, but may lack liability protection.
- Limited Liability Company (LLC): Popular for protecting personal assets with tax flexibility.
- S-Corporation: A tax election for an LLC or corporation to avoid double taxation.
- Professional Corporation (PC/PLLC): Required in many states for licensed professionals, offering business liability protection.
After choosing a structure, register your business with the state and get a federal Tax ID Number (EIN) from the IRS, which you can apply for an EIN online. If you're forming your business in 2024 or later, you must also file a Beneficial Ownership Information (BOI) report with FinCEN. Finally, open a dedicated business bank account to keep finances separate from day one.
Phase 2: Licensing, Location, and Physical Setup
With your plan in place, it's time to handle the legal necessities and find a physical home for your practice. This phase involves navigating regulations and designing a space that is welcoming to patients and efficient for your team.

Obtain Mandatory Licenses, Permits, and Certifications
This step is non-negotiable and can take months, so start early. It's a critical item on your checklist for starting a new medical practice. You will need:
- State Medical Board License: Your permit to practice medicine in the state.
- DEA Registration: Required to prescribe controlled substances.
- National Provider Identifier (NPI): A unique ID for all healthcare providers.
- CLIA Waiver/Certification: Needed for any on-site lab testing.
- Local Business Permits & Certificate of Occupancy: Required by your city or county.
Additionally, you must ensure compliance with OSHA for workplace safety and HIPAA for protecting patient health information. Delays in this area can postpone your opening and be costly.
Select and Set Up Your Physical Office Space
Your location is a key factor for patients. When scouting locations, consider patient demographics, accessibility (including parking and ADA compliance), visibility, and proximity to potential referral sources. Also, verify local zoning regulations permit a medical practice.
Next, decide between leasing vs. buying. The best choice depends on your financial situation and long-term goals.
| Feature | Leasing | Buying |
|---|---|---|
| Upfront Cost | Lower (security deposit, first month's rent) | Higher (down payment, closing costs) |
| Flexibility | More flexible for relocation or expansion | Less flexible, but can be a long-term asset |
| Control | Limited control over property modifications | Full control over design and modifications |
| Equity | No equity building | Builds equity, potential for appreciation |
| Maintenance | Often handled by landlord | Your responsibility (or property manager's) |
| Long-Term Cost | Rent increases over time | Mortgage payments can be stable, tax benefits |
Leasing is common for new practices due to lower upfront costs. Regardless of your choice, have an attorney review any agreement. For the office layout, prioritize an efficient patient flow, a welcoming waiting area, private exam rooms, and an administrative space. Ensure everything is ADA-compliant. Consider hiring a healthcare architect to optimize the space for growth.
Handle Credentialing and Contracting with Insurance Providers
This is often the most time-consuming part of the setup. Credentialing is the process where insurance companies verify your qualifications. It can take 90 days or more per payer, so start as early as possible. You'll need to complete payer enrollment with Medicare, Medicaid, and all commercial insurance plans you intend to accept. Many practices hire a professional credentialing service to manage this complex process.
Finally, secure the right insurance for your practice itself. This includes non-negotiable malpractice insurance, general business liability insurance to cover accidents on your property, and property insurance for your building and equipment.
Phase 3: Operations, Staffing & Technology
Now it's time to build the internal engine of your practice. This part of your checklist for starting a new medical practice focuses on creating efficient workflows, implementing technology, and hiring the team that will deliver outstanding patient care.

Build Your IT Infrastructure and Select Equipment
A secure and robust technology backbone is essential for modern healthcare. Your Electronic Health Record (EHR/EMR) system is the digital heart of your practice, managing patient charts, prescriptions, and clinical notes. Choose a user-friendly system that is specialty-specific if needed. Your practice management software, which often integrates with the EHR, handles scheduling, billing, and financial reporting.
A patient portal is now an expected convenience, allowing patients to schedule appointments, view results, and communicate with your office online. Furthermore, since surveys show 83% of U.S. patients expect to continue using telehealth post-pandemic, integrating a secure telehealth platform is crucial for attracting and retaining patients.
IT security is paramount. Implement strong firewalls, data encryption, and regular backups to ensure HIPAA compliance and protect sensitive patient data. Also, invest in reliable, high-speed internet and a professional phone system. For medical equipment, create a comprehensive list based on your services, source from reputable suppliers, and consider group purchasing organizations for discounts.
Assembling Your Team: A Critical Part of the Checklist for Starting a New Medical Practice
Your staff is the face of your practice. Start with a staffing needs assessment based on projected patient volume. Key roles include:
- Practice Manager: Oversees daily operations, staff, and billing. Often the most critical first hire.
- Nurses (RNs/LPNs): Provide clinical support and patient education.
- Medical Assistants: Handle patient intake, vitals, and administrative tasks.
- Front Desk Staff: Manage scheduling and are the first point of contact for patients.
Develop clear job descriptions and conduct a thorough hiring process, including background checks. Once hired, provide comprehensive onboarding. Set up payroll services and create a detailed employee handbook covering policies, benefits, and compliance guidelines for HIPAA and OSHA. Fostering a positive work environment from day one is key to reducing turnover.
Establish Operational Systems and Policies
Streamlined operations are the key to a successful practice. Define clear workflows for every patient touchpoint.
- Appointment Scheduling: Choose a system (e.g., block scheduling) and train staff thoroughly.
- Patient Registration: Create a smooth intake process with all necessary forms (registration, medical history, consent, HIPAA notice).
- Billing and Collections: Define a clear workflow for charge entry, claims submission, and collections. Many practices outsource medical billing to increase net revenue.
- Medical Records Management: Establish protocols to ensure accurate and confidential records within your EHR.
- Compliance Manuals: Your HIPAA and OSHA manuals should be living documents that guide daily practice and staff training.
- Office Policies & Emergency Plan: Develop policies for patient conduct and cancellations, and create an emergency preparedness plan for situations like fires or natural disasters.
Phase 4: Launch, Marketing, and Sustainable Growth
You've built the practice; now it's time to attract patients and plan for long-term success. This final phase is about marketing, ensuring continuity of care, and positioning your practice for sustainable growth.
Market Your New Practice and Build Your Patient Base
Effective marketing is crucial for patient acquisition. Start with practice branding by developing a professional logo and a clear message. Learn more about branding for doctors. Your professional website is your digital front door; it must be mobile-friendly and contain key information like services, insurance, and contact details. Claim and optimize your Google Business Profile, as over 65% of U.S. patients check online reviews before choosing a doctor.
Use social media platforms like Facebook or Instagram to share health tips and connect with your community. Build referral relationships by acting as a physician liaison and networking with other local providers. Explore digital marketing for doctors, including online ads and SEO, to expand your reach. Finally, a grand opening event can create local buzz. Find more healthcare advertising ideas to get started.
Plan for Continuity of Care and Physician Well-being
Practice ownership is demanding, and preventing burnout is essential. As one expert notes, it is "absolutely essential to ensure that your practice model will allow you to take time off." Plan for how patients will be cared for when you are unavailable.
Call coverage solutions include forming a call group with local peers, using locum tenens services for planned leave, or making cross-coverage agreements with other practices. Telemedicine can also help manage after-hours inquiries. Actively plan for your own vacation and sick leave. Delegate tasks, build a work-life balance, and use resources from organizations like the American Medical Association. You can find valuable AMA resources on practice management.
Consider Ancillary Services and Advanced Practitioners
As your practice grows, consider expanding your offerings to improve patient care and increase revenue. Hiring Physician Assistants (PAs) and Nurse Practitioners (NPs) can boost your capacity, allowing you to see more patients. Be sure to understand your state's scope of practice laws and supervision requirements.
Offering ancillary services like in-house labs, diagnostic imaging, or physical therapy can make your practice a convenient one-stop shop. However, these services require significant upfront investment, additional regulatory compliance (like CLIA certification), and increased administrative work. Before adding them, conduct a thorough market analysis to confirm patient demand and financial viability. Get more insights by analyzing healthcare market competition.
Frequently Asked Questions about Starting a Medical Practice
It's natural to have questions when starting a medical practice. Here are answers to some common queries from physicians.
Should my new practice hire Physician Assistants (PAs) or Nurse Practitioners (NPs)?
Hiring PAs or NPs can be a smart move. They can handle a wide range of primary care duties, which increases patient access and frees you to focus on more complex cases. They are also a cost-effective way to expand your team. However, you must understand and adhere to your state's specific scope of practice laws and physician supervision requirements. The decision should align with your patient care model and growth strategy.
How can a solo or small practice handle call coverage and prevent burnout?
For solo and small practices, strategic planning is key to preventing burnout while ensuring continuous patient care. Effective strategies include:
- Forming a Call Group: Partner with other local physicians to share after-hours and weekend call duties.
- Using Locum Tenens Services: Hire temporary physicians to provide coverage during vacations or extended leave.
- Establishing Cross-Coverage Agreements: Create formal agreements with nearby practices for mutual support.
- Leveraging Telemedicine: Use a secure telehealth platform for after-hours consultations to reduce the need for in-person visits.
Prioritizing efficient practice management and scheduling dedicated time off are also crucial for your well-being and the long-term success of your practice, making it a vital part of your checklist for starting a new medical practice.
Is it a good idea to offer ancillary services from the start?
Offering ancillary services like in-house labs or imaging can diversify revenue and improve patient convenience. However, for a new practice, the challenges can be significant. These services require a large upfront investment in equipment and space, involve additional regulatory compliance (e.g., CLIA certification), and increase administrative overhead. Before investing, a thorough market analysis is crucial to confirm patient demand.
For most new practices, the best advice is to focus on establishing your core services first. Once your practice is stable and you have a clear understanding of your patient base, you can strategically introduce ancillary services that align with your vision.
Conclusion
Starting a new medical practice is a complex but rewarding journey that blends clinical expertise with an entrepreneurial spirit. While challenges are inevitable, every successful independent physician has steerd this path. This checklist for starting a new medical practice provides a roadmap to break the process into manageable steps.
Careful planning and methodical execution are the keys to your success. The time invested in building solid systems, hiring the right team, and establishing efficient workflows from day one will pay dividends. Most importantly, stay focused on providing excellent patient care while building a sustainable business.
The autonomy you gain is unparalleled. You will have the freedom to practice medicine as you envision it, creating something truly meaningful for your patients and community.
At Digital Ash Agency, we understand the unique challenges physicians face, from navigating competitive markets to dealing with non-compete restrictions. We help you craft your brand story, build your online presence, and attract your ideal patients.
Your dream of independent practice is within reach. With this roadmap and the right support, you are ready to take the next step.








